
Imagine how the already pressed world of primary care nursing would cope without 20% of its most experienced clinical staff. Driven from the profession by a process actually intended to improve it.
This could be a real possibility as new research from Independent Nurse has found that a fifth of nurses have considered retirement rather than revalidation.
In a survey answered by 508 primary care nurses, nearly 20% said either they would retire early or knew of colleagues who would exit the profession rather than engage with the painstaking record-keeping, study days and written work now required. Given that 47% of respondents to the survey were over 55, this could be a reality as the new model of revalidation begins in April 2016.
One respondent said: ‘I know two very experienced nurses who are working past the national retirement age, who are excellent and provide professional expertise to patients and colleagues. They will not be renewing their registration when it’s due because of the stringent requirements for revalidation.’
Another said: ‘I will be 60 when I am due to revalidate. Although I planned to stay on after this date I have now decided to retire.’
To their credit nursing leaders are alert to the danger. Speaking at the Primary Care Nursing Expo (PCN Expo) on 3 February Jackie Smith, the Nursing and Midwifery Council’s (NMC) chief executive, acknowledged that there is a risk that nurses may choose retirement over revalidation.
‘I think the more that you see the benefits of revalidation nurses and midwives hopefully won’t take that decision to retire rather than go through the process,’ she said.
Howard Catton, the head of policy and international affairs at the Royal College of Nursing (RCN) says that these results should not be ignored. ‘I think we need to acknowledge that if we don’t communicate this well and set out revalidation simply and clearly, there is a risk that people will think it’s more difficult than it is. People could say that they will retire and they will not revalidate,’ he says.
Mr Catton says that the NMC collects data on how many nurses drop off the register every month based on a number of reasons such as retirement, career change and moving abroad. ‘The NMC should monitor the number of drop offs around the the time of revalidation. If there is an increase in the number of people not re-registering then the NMC can identify that early,’ he says,
‘If necessary they could do some follow-up work with those individuals to ask what the reasons were and if they were part of a particular age group or setting and whether it was down to revalidation or not.’
The Queen’s Nursing Institute (QNI) recently surveyed 3405 nurses and collated the results in a report: General Practice Nursing in the 21st Century: A Time of Opportunity.
When asked how they felt about revalidation encouragingly 80.7% of respondents said they would be able to meet the requirements.
However, some respondents had expressed that they were exploring the option of early retirement. ‘I need to know more about what’s expected and work out how I am going to manage my time and commitments to meet the requirements necessary to revalidate. I have also been looking at early retirement or reducing my hours,’ one answered.

Setting setback
Age was not the only concern that respondents felt around revalidation. Over half did not feel that revalidation will cater sufficiently for nurses in primary care or that the NMC had sufficiently explored how revalidation would work for primary care nurses.
Around 60% felt the process wasn’t suited for nurses in primary care. One respondent answered that the pilots were ‘weighted towards nurses working within a large organisation such as hospitals. If it is going to work properly a “one size fits all” approach won’t work. The requirements should be tailored to the area in which you work.’
One of the most common answers given for why it wouldn’t work for primary care was because many nurses work in single nurse GP surgeries so would not have as many opportunities to reflect with other nurses.
‘Many work in isolation and do not have the support of other nurses around them. Some nurses are not allowed much time to attend study days or given protected time,’ said one respondent.
Another respondent said: ‘Sole nurses working in remote areas will struggle to get another NMC member to confirm. I work as a lone nurse and I will find it very difficult to get someone to confirm for me.’
Interestingly the comments outlining the nurses’ anxieties around the revalidation mirrored those expressed in the QNI survey too. These included having the time to complete the portfolio, having enough time for CPD, working in isolation and not having a senior nurse to act as a confirmer.
In response to these findings Maureen Baker, chair of the Royal College of GPs, said the increasing number of consultations was being felt by practice nurses. ‘It is concerning that as a result of these pressures, practice nurses do not feel they have the capacity to adequately prepare for revalidation or complete continued professional development.
‘It is important that practice nurses receive the best possible education, training and support in order to do their job well, and help keep our patients safe,’ she says.
Almost 80% of the respondents thought the pilots were not representative of nurses in primary care and over 200 of the respondents were unaware revalidation pilots had taken place in primary care or did not feel that they had seen enough evidence from the pilots.
Independent Nurse reported that the first wave of pilot sites was announced in October 2014 and that GP practices were identified in the second wave of pilots in November 2014.Nursing leaders reacted with concern to our findings.
‘We shouldn’t ignore that people are telling us that they weren’t aware of the pilots,’ says Mr Catton. ‘I think it probably tells us that we need to do more to share with those people, that we know and understand what the issues are specifically for them. Perhaps there is a need for more targeted communication for this group.’
One respondent said that GP practices appear to be relatively disinterested in revalidation, and another said that the pilots had been ‘weighted towards larger organisations like hospitals’.
However, one respondent was aware of pilots that had happened in local GP practices and said that ‘many of the nurses felt [the pilot] was very helpful’.
This contrasts to another respondent who was part of a pilot and said: ‘I wouldn’t know. There was zero feedback. After putting a significant amount of effort into being part of the pilot, I heard nothing. Very disappointing.’
But Katerina Kolyva, the director of continued practice at the NMC, said the revalidation pilot covered a wide range of settings and scope of practice. ‘Across the UK, over 30% of those that participated in the revalidation pilots said they worked in a primary care setting,’ she says.
Employer prep
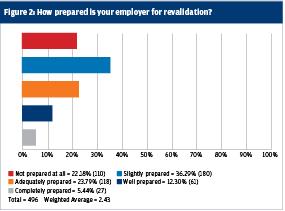
There were varying answers when the nurses were asked if their employers were prepared for revalidation. Nearly 60% of employers are not adequately prepared to support nurses for revalidation.
Only 5.3% said they didn’t have any concerns around revalidation. Around 30% of the respondents felt they wouldn’t be given enough enough time to complete the portfolio or wouldn’t be given the time to carry out CPD.
Other issues from the respondents were getting their portfolios right, the amount of extra work that they would have to undertake and getting their head around the technological side.
Some were concerned that it would be difficult to complete the portfolio on their home computers or accessing work documents held in their practice intranets would hinder them. As nearly 90% of the respondents were over 45, it was also notable that a high percentage of them stated that they didn’t feel confident to record their portfolios electronically.

However, despite the levels of concern revealed by this survey 58% felt that the process would be positive for nursing and that it would benfit their careers. Some respondents stated that it would be a way for nurses to reflect on their own practice and hold nurses more accountable for their work. Some respondents also stated that revalidation would improve public perception of the nursing workforce.
‘It will be a record of my work and the quality of work I have done,’ answered one respondent. Another said that it will ‘allow me to plan my career pathway and where I need to upgrade my own skills to safely administer care in whichever field I continue to practice’.
Whether nurses like it or not, revalidation becomes a reality this spring. From April 2016 up to 30,000 nurses are due to revalidate.
The NMC’s best piece of advice so far is that should a nurse have any concerns they should either visit the website or call the NMC helpline. A guided entry to the brave new world of revalidation might prove much easier than simply deciding to leave a profession you love.

| What you need to know about revalidation |
|
Resources
1. NMC website. http://revalidation.nmc.org.uk
2. The RCN. https://www.rcn.org.uk/professional-development/revalidation.
3. The Queen’s Nursing Institute. General
Practice Nursing in the 21st Century: A Time of Opportunity. January 2016.
