
When a patient presents with worries about their liver, the natural response for a nurse is probably ‘put down the bottle’. Increasingly, the right message might be ‘put down the fork’.
Non-Alcohol related Fatty Liver Disease (NAFLD) is already the most common liver problem in the western world with 20-30% of the population affected,1 the vast majority undiagnosed. Just last month, it was linked strongly to type 2 diabetes by a study from the University of Edinburgh.
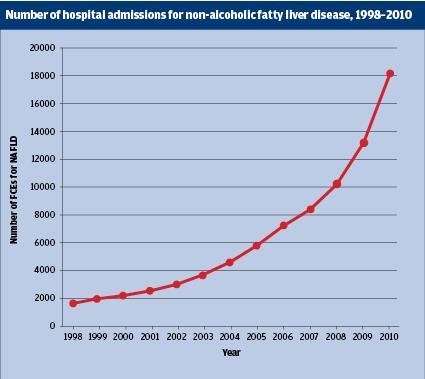
‘In a nutshell, we’re facing an epidemic of NAFLD in the UK in the same way as has been experienced in the United States,’ says Andrew Langford, chief executive of the British Liver Trust and a registered nurse. ‘There has been a significant rise, certainly in the last 10 years in NAFLD. The biggest problem in the UK is the double whammy of people who are at risk of NAFLD but are also drinking too much. That doesn’t just double your chances of liver disease, it’s roughly 18 and 20 times more. There’s a huge issue with both risks of NAFLD and the rise is very similar to that of type 2 diabetes.’
According to the Lancet Liver Campaign,2 liver disease in the UK stands out as ‘the one glaring exception’ to the vast improvements made during the past 30 years in health and life expectancy for chronic disorders such as stroke, heart disease, and many cancers. Overall mortality rates have increased by 400% since 1970, and in people younger than 65 years by almost 500%.
The condition is the third most common cause of premature death in the UK, with the All-Party Parliamentary Group on Liver Health predicting that it is has ‘the potential to become the UK’s biggest killer within a generation.’ The rate of increase of liver disease is substantially higher in the UK than other countries in western Europe.
While alcohol is still the biggest culprit of all the liver disorders that lead to this severe liver damage, NAFLD is quickly becoming the most common.
‘Liver disease is a huge burden on the NHS and a major cause of premature death in the UK,’ says Lynda Greenslade, clinical nurse specialist in hepatology at Royal Free Hampstead NHS Trust. ‘Nursing staff have the potential to ease this problem, but they need the skills and competence to tackle liver disease head-on.’
The rise of NAFLD, which in many cases leads to more severe liver disease, is down to skyrocketing rates of obesity. With 25% of the population now categorised as obese, the spread of NAFLD has been alarmingly. It is estimated that one in five people2 in the UK have NAFLD, and many will have ongoing inflammation and scarring that finally leads to cirrhosis. Of those patients with cirrhosis, 5–10% will get liver cancer.
‘The increase in mortality means we have over 40 people a day dying a day in the UK. that seems ridiculous when 95% of liver disease is preventable. One the one hand, there is an awful lot of pressure on the service delivery in the NHS but there’s very little preventative work going on,’ says Mr Langford.
The result is not just bad for the nation’s health, but for its wallet as well. The cost to the NHS is estimated to be £4.2 billion3 and is projected to double that by 2050.‘NAFLD is putting significant pressure on NHS services. Not only is it it resulting in a long term condition, it also means that demand for things like liver transplants is a lot higher, the need for long term care is a lot more, acute care, or general healthcare management,’ says Mr Langford.
Amanda Cheesley, the professional lead for long term health conditions at the RCN, says it is crucial for the condition to be diagnosed early. ‘In a similar way for health conditions related to obesity, there additional pressures on the NHS created by liver,’ says Ms Cheesley. ‘If you diagnose it reasonably early then it is isn’t so costly, but often the potential of liver disease isn’t diagnosed early because you have to do a liver function test to identify it.
There is an overemphasis on looking at people’s blood glucose levels and not necessarily considering if the liver has any damage. If it isn’t caught early, its another nasty life threatening disease.’
Prompt diagnosis really can make a difference as the liver has exceptional regenerative powers.
‘The good news is if we catch NAFLD early enough, and there are some lifestyle changes, then you can have a significant effect on the long-term health of your liver,’ says Mr Langford.
There is no specific treatment for NAFLD agreed on by the medical establishment, but as the condition is linked to being overweight then it is advisable for patients to make lifestyle changes including losing weight gradually and taking exercise. There is evidence that gradual weight loss coupled with increased exercise can reduce the amount of fat in your liver.3
In mild cases, healthcare professionals should concentrate on treating associated conditions, such as obesity and diabetes.
A recent report by the Lancet Commission2 emphasised identified the need for much earlier detection of liver disease by GPs. The report also suggested that there was a ‘postcode lottery’ with treatment of NALFDs. ‘In some places, if you’re lucky there are liver wards, but in most hospitals that will be a general ward, and care and management can be very intense,’ says Mr Langford.
As NAFLD is a largely symptomless disease, it may be difficult to detect. ‘There are two things that are very easy to do. One is that if you are doing a health check, or you have somebody standing in front of you, don’t just do a BMI, although that’s helpful to identify the overweight,’ says Ms Cheesely. ‘You need to do a waist circumference check. That is a far better indicator that there may be fatty deposits around the liver. In particular, people with round stomachs should have the check.’
‘If you think there may be a risk, do a blood test, particularly if someone is in a health check, because you’re going to be checking for cholesterol. So include a liver function test too. That’s especially important for nurses in a practice environment,’ she adds.
Mr Langford agrees that the need for better screening is vital in combatting the damage done by NAFLD. ‘We have a ridiculous situation where we still don’t test all people with type 2 diabetes for their liver function. That’s crazy. Knowing that they go hand in hand, it should be compulsory that people have their liver function tested on a regular basis.’
A project piloted by Hull and East Yorkshire Hospitals NHS Trust aimed to address the issue of appropriate referral. It brought together general practices and liver specialists through an e-consultation clinic, as part of an IT-based integrated care pathway for NAFLD. The e-consult pathway standardised care by detailing necessary investigations to determine the cause and severity of liver disease, and promotes early and accurate diagnosis. Patients presenting in primary care with abnormal liver function tests will be entered onto the e-consult pathway. Practitioners can make a referral decision: to manage the patient in primary care or refer them to a specialist.
‘Nurses are integral to making an impact on liver disease; nurses can make every contact count by identifying risk factors for the three major types of liver disease – alcohol, hepatitis B and C and obesity leading to non-alcoholic fatty liver disease,’ says Michelle Clayton, lecturer in liver care at the University of Leeds.
‘I think particularly for nurses there is a great role to play. No matter where you work as a nurses, there are opportunities in both primary and secondary care,’ says Mr Langford. ‘If you have a patient who is overweight or obese, you can have a conversation, but its also about making sure that the patient has the right blood test or scans, just to see what the health of their liver is.’
As the problem of NAFLD increases, nurses will have to be able to identify its sufferers. Maybe the liver function text should become as ubiquitous as the blood pressure check in our practices.
Resources
British Liver Trust. Love your liver health screener. loveyourliver.org.uk/love-your-liver-health-screener
References
1. British Liver Trust. Facts about liver disease.http://www.britishlivertrust.org.uk/about-us/media...
2. The Lancet. The Lancet Liver Disease Campaign.http://www.thelancet.com/journals/lancet/article/P...
3. British Liver Trust. Non alcohol related fatty liver disease. http://www.britishlivertrust.org.uk/liver-informat...
What do you think? Email your view to IN@markallengroup.com or tweet @IndyNurseMag
