
Almost 43,000 people are diagnosed with bowel cancer every year in the UK. More than nine out of ten new cases (94%) are diagnosed in people over the age of 50. But bowel cancer can affect anyone at any age.1
Recognising the critical importance of early diagnosis in saving lives, especially with diseases like bowel cancer which can be effectively treated if detected at its earliest stage, both NHS England and the Government have pledged to achieve a 75% early-stage cancer diagnosis rate by 2028.
Sharp rise in bowel cancer in under-50s
Why we need to talk about bowel cancer
Identifying and managing irritable bowel syndrome
In primary care settings, patients frequently exhibit a wide array of bowel symptoms, spanning from mild discomfort to potentially life-threatening conditions. Distinguishing between serious ailments such as cancer and more benign issues like haemorrhoids can pose a significant challenge. Central Camden PCN, covering nearly 100 000 patients, has taken a proactive step in answering this challenge by introducing a dedicated community rectal pathology clinic at Bloomsbury Surgery in North London. The surgery, part of Central Camden PCN, is medium sized, and we have 8400 registered patients. It is easily accessible by all patients registered within the PCN.
According to the current guidance from NICE, individuals presenting with low-risk symptoms indicative of colorectal cancer in primary care settings are recommended to receive FIT. Conversely, those exhibiting high-risk symptoms should be swiftly referred to the suspected cancer pathway. However, capacity constraints often lead to prolonged waiting periods for colonoscopy, exacerbating the issue.
NHS waiting times at record time for bowel patients
The number of people waiting more than a year-and-a-half for NHS treatment in England is rapidly growing and has hit a record high . New performance data on referral to treatment (RTT) shows patients waiting to start treatment at the end of November 2023 was 7.6 million. Among this 7.6 million, there are almost half a million people waiting over 50 weeks and around 100,000 waiting over 60 weeks.2,3
In our PCN, we were seeing patients with low-risk colorectal issues waiting up to 70 weeks for treatment in secondary care. This is because even if we think the patient is suffering with haemorrhoids, we would still need a bowel expert to check the bowel to rule out something more serious – like cancer – before the haemorrhoids are treated. While not life-threatening, they can still be life-limiting. They may affect someone’s ability to sit for extended periods of time and can cause significant pain and worry.
New technology is key to clinic’s success
The clinic owes its operational capability to the recent acquisition of a cutting-edge British medical technology; a digital rectoscope called LumenEye X1. It can get a clear view of the inside of the lower part of the bowel. Giving a direct visualisation of the anorectal tract in the general practice setting, can quickly identify what the problem might be - either eliminating the need for formal endoscopy or identifying cases that require a colonoscopy due to polyps or other serious pathology being found – simultaneously reducing the burden on endoscopy services and improving the diagnosis of cancer in patients who do not meet the criteria for urgent referral.
The pioneering new device’s HD camera creates high quality images and videos of the lower bowel (up to 18cm from the anus), aiding the team in spotting rectal cancer as well as diagnosing other bowel concerns such as inflammatory bowel disease and haemorrhoids. It reduces costs of unnecessary investigations into benign disease, all while supporting NHS goals to create diagnostic hubs in the community, improve the patient experience and health outcomes, whilst taking pressure off over-stretched endoscopy departments in hospitals.
The LumenEye has recently been prioritised by NHS England as a technology for lower gastrointestinal diagnostic pathway development within community diagnostic centres.
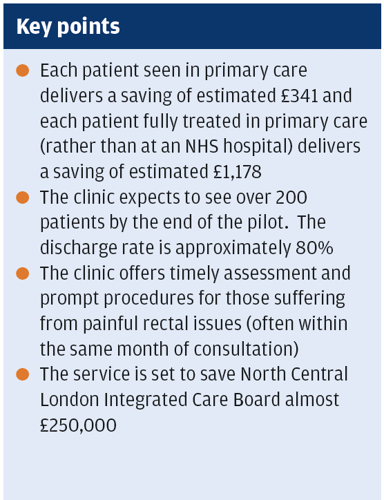
The clinic has seen a discharge rate of around 80%; this means patients (usually those with painful rectal issues) are having procedures done in the clinic in the same month. Benign diseases of the bowel can have a big impact on quality of life and as clinicians we want people to be treated as expediently as possible.
Barriers to diagnosis and treatment
As GPs we know that cervical screening is frequently avoided by women. For many people investigation for bowel issues are embarrassing and avoided, but there may also be cultural reasons why a woman does not want to speak to or be examined by a male healthcare professional.
In our PCN, we have patients from diverse backgrounds and we understand the cultural barriers for many women who are suffering from bowel complaints. When setting up the service we were very keen to be able to offer a female practitioner and one of our allied healthcare professionals Vidhi Patel, has been trained to use the LumenEye device and offer consultations. Having a female practitioner is wonderful to have to be able to help these women who may have refused treatment from a male doctor.
I also think that being seen in a local GP surgery room, is far less daunting than a hospital. There is not the worry that comes when you are waiting several months for colonoscopy. After speaking to the GP most patients can be seen at the rectal pathology clinic within a couple of weeks. There is also not the stress of using bowel prep or fasting, as comes with colonoscopy. Patients need only use a suppository before coming into clinic.
A successful pilot here in London
The clinic represents an innovative approach to improving access to colorectal healthcare services, particularly for patients with lower-risk gastrointestinal symptoms. Our practice staff take on expanded roles in the assessment, diagnosis, and management of bowel-related concerns under the supervision of general practitioners (GPs) or gastroenterologists. The clinic is funded by the PCN (Camden Health Evolution), the North Central London Cancer Alliance and UCL Partners. The PCN fund the staff and capital, while receiving some funds from UCLH to support consumables, and the LumenEye device has been loaned by medical device company SurgEase for the period of the pilot.
The PCN’s initiative is revolutionising patient care in primary healthcare by providing prompt and efficient services while easing the burden on London’s overstretched NHS colorectal departments.
I aspire for the UK to set a shining example by creating a resilient and streamlined digital cancer pathway. Through this initiative, we anticipate a reduction in the significant regional differences in cancer outcomes, often termed the ‘postcode lottery’, ensuring that patients are efficiently directed into appropriate cancer care pathways at the moment of need. By establishing community clinics led by proficient GPs, augmented with virtual specialist guidance for thorough diagnostic evaluation, we aim to detect cancers at their onset, facilitating earlier diagnoses and timely treatment interventions.
Dr Ammara Hughes, General Practitioner, Bloomsbury Surgery and Clinical Director, Central Camden PCN
1. Bowel Cancer UK. Facts and figures about bowel cancer. Available at: https://www.bowelcanceruk.org.uk/about-bowel-cancer/bowel-cancer/#:~:text=Almost%2043%2C000%20people%20are%20diagnosed,affect%20anyone%20of%20any%20age.
2. The Standard. NHS waiting list hits record high of 7.77 million. Available at: https://www.standard.co.uk/news/uk/nhs-waiting-list-record-high-a-and-e-figures-tories-rishi-sunak-b1119222.html
3. NHS England. Statistical Press Notice NHS referral to treatment (RTT) waiting times data November 2023. Available at: Nov23-RTT-SPN-Publication-PDF-442K-61260.pdf (england.nhs.uk)
