
The beginning of 2017 heralds the release of yet another report highlighting where the NHS could improve.
These reports come thick and fast from many different organisations and health bodies, but recommendations are often slow to be taken up.
This time it is Asthma UK’s 2016 annual survey.1 Results reveal that 82% of the 4650 respondents felt that their asthma was poorly controlled and more than a quarter missed a week or more of work or education a year because of asthma exacerbations. These results are very similar to those in last year’s Asthma UK report.
However, a third of people now say they receive basic asthma care, an increase on the 28% reported last year. While this increase is welcomed, the flip side is that two thirds of people are still not receiving basic asthma care.
Dr Andy Whittamore, GP and clinical lead at Asthma UK, suggests that some of this may be down to the fact that many healthcare professionals are having to fit more into shorter and shorter consultation times.
‘I now see someone for just 10 minutes and so I try and fit in as much information as I can. I will then try to signpost [the patient] to where they can find more information on the condition,’ he said.
Dr Whittamore also said that many patients can become complacent about asthma and this can lead to uncontrolled symptoms. The role for the healthcare professional in overcoming patient complacency is to reinforce the importance of self care in asthma.
‘We have got a lot of work to do to educate people with asthma and healthcare professionals about the importance of recognising the symptoms, linking the symptoms to the underlying inflammation and associating that with the risk of future events,’ he says.
The survey asked respondents whether they had been hospitalised or accessed out-of-hours care and just 29% of respondents said they had. However, 70% of this cohort said that they did not receive a follow up appointment with a GP or practice nurse.
These results are in line with the National Review of Asthma Deaths released in 2014,2 which found that two-thirds of people who were hospitalised in the month before they died did not receive the necessary follow-up care.
‘Despite two years having passed since NRAD’s publication, there are still thousands of people with asthma not receiving the correct treatment following a potentially life-threatening episode,’ the report says.
Despite this, 85% of people with asthma are exclusively managed in primary care.1
Natalie Harper, a respiratory advanced nurse practitioner and executive committee member of the Association of Respiratory Nurses, says that one of the key ways of improving patient experience is to ensure that all clinicians have asthma management education and to ensure that there is greater communication between primary and secondary care. This would lead to more patients having follow-up consultations with their GP or practice nurse.
Ms Harper also states: ‘An awful lot of GPs will hold their hands up and say that most of the chronic disease management is done by the nurses in primary care, therefore [the GPs] are not necessarily up to date with what should be done.’
More education would ensure that more clinicians understand the importance of personal action plans. The survey identified that 42% of respondents now receive asthma action plans, almost double the proportion (24%) who received them in 2013.
A written asthma action plan can mean that a patient is four times less likely to be admitted to hospital for asthma related exacerbations. Ms Harper says that the rise in personal action plans is encouraging.
Local variations
As is the case for many other conditions, there were local variations noted in the report. The most prominent was the fact that just 27.5% of people in London received basic asthma care compared with 47.6% respondents in Northern Ireland. The area with the second highest rating was the North East with 38.5%.
Dr Whittamore says that it is difficult to pin down exactly why the variations are so vast between areas but offers a few explanations of why this could be the case.
‘London has a more transient population than other areas, and there is a higher percentage of ethnic minorities.’
He adds: ‘It is also more difficult to get a GP or practice nurse appointment in London than it could be in other places. I’m sure this is all part of the reason.’
Ms Harper thinks that the lack of financial investment following the release of documents such as the Asthma UK report is the main reason change doesn’t occur.
‘I know everywhere is struggling with funding and the impact of austerity measures over the years but there’s got to be some funding put in place from government level to actually implement some of these changes if they are going to be done properly for the patients benefit,’ she says.
Prescriptions
Another barrier to good asthma management identified in the report was prescription charges.
Nearly half (46%) of the respondents stated that paying for prescriptions impacted on their ability to pay for other activities.
Asthma UK believes that ‘more can be done to relieve this burden of payment’. The charity states that it will continue to campaign for changes in prescription costs as part of the Prescription Changes Coalition.
In relation to medication management for asthma patients NICE is currently consulting on draft guidance which will change the way medications are prescribed if it goes through.
The consultation recommends that patients are offered leukotriene receptor antagonist (LTRA) tablets before they are offered the combination inhaler. The tablet costs the NHS seven pence a day and could ultimately save the NHS millions if the guidance is accepted.
‘The evidence for combination inhalers and LTRAs shows that they are both clinically effective when used as a step-up treatment. Due to its lower price, NICE’s independent guideline committee concluded that LTRA was significantly more cost-effective and would be better value for money for the NHS,’ says the consultation document.
Ms Harper says that the introduction of new NICE guidance into asthma care could confuse clinicians as the BTS/SIGN guidelines already exist. ‘It would be better if NICE and BTS/SIGN worked together to create one guidance. Or, even if there are two sets of guidance to have the same information covered in both.
‘GPs and practice nurses have a lot of conditions to keep on top of, so may struggle to keep up to date with [them], so I think it’s going to cause a lot of problems if there are two lots of guidance talking about different things [in relation to asthma],’ she says.
The annual Asthma UK survey provides valuable data on the state of asthma care now. However, while the collection of data is key to identifying issues, they should then be used as a catalyst for change. ‘Reports like these are great and they raise a lot of questions as well as answers, but if there is no funding to put some of these things in place patient care won’t get better,’ concludes Ms Harper.
References
1. Asthma UK. Annual Asthma Survey. 2017. https://www.asthma.org.uk/globalassets/get-involved/external-affairs-campaigns/publications/annual-asthma-care-survey/annualasthmasurvey2016final.pdf.
2. Royal College of Physicians (RCP). 2014. Why asthma still kills: The National Review of Asthma Deaths (NRAD).
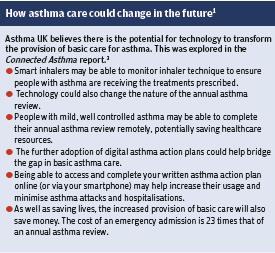
3. Asthma UK. Connected asthma: how technology will transform care. 2016. https://www.asthma.org.uk/globalassets/get-involved/external-affairs-campaigns/publications/connected-asthma/connected-asthma---aug-2016.pdf.
