
Chronic Obstructive Pulmonary Disease (COPD) is a chronic, debilitating and progressive disease with many patients having frequent exacerbations requiring intervention.1 COPD incorporates a variety of diseases including emphysema and chronic bronchitis and has irreversible chronic obstruction of airflow, with smoking being the primary causation in 80% of patients.2 Symptoms can include increased shortness of breath, sputum production, weight loss and restricted mobility which can vary in severity and may affect all aspects of daily living. The severity of COPD is commonly classified based on the GOLD (Global Initiative for Chronic Obstructive Lung Disease) criteria.3 It is based on comparing the measured forced expiratory volume in 1 second (FEV1) against the predicted value. It classifies patients into four categories: mild; moderate; severe; and very severe. In patients with FEV1/FVC <70%:
- GOLD 1 (FEV 1>= 80% predicted)
- GOLD 2 (FEV 1 50-79% predicted)
- GOLD 3 (FEV 1 30-49% predicted)
- GOLD 4 (FEV <30% predicted)
Common medical management may include bronchodilators (inhalers, nebulisers) which may also be used in conjunction with agents such as: oral mucolytic therapy; corticosteroids; oxygen therapy; and long-term antibiotics and are often managed by either the General Practitioner (GP), specialist respiratory nurse or by respiratory physicians. Smoking cessation and pulmonary rehabilitation may be advised in conjunction with pharmacological interventions, to optimise the breathing of individuals.
The disease spectrum can progress in patients to advanced emphysema where the destroyed lung hyper expands, impeding gas exchange. Over a period of time this can also lead to flattening of the diaphragm and hyper expansion of the chest (barrel chest) impeding respiratory mechanics.
For some patients in addition to the above measures, lung volume reduction (LVR) may be an additional treatment that could be explored. Although surgical intervention for patients with emphysema could be beneficial in selected patients, not all suitable patients are being referred
for LVR.
This possibly reflects clinicians being unsure which patients should be referred and ambiguity about when to refer, or could be related to the clinicians’ personal preference or scepticism about the efficacy of the procedure, combined with patient misinformation.
Investigations in decision making
Patients require:
- Full lung function tests including plethysmography which enables assessment of significant airflow obstruction (forced expiratory volume in 1 second (FEV1) 20-40% predicted); significant hyperinflation total lung capacity (TLC) >120% predicted, residual volume (RV) >180% predicted and transfer factor >40%.
- High Resolution Computed Tomography (HRCT) to assess heterogeneous emphysema pattern and integrity of interlobar fissures (>90%).
- Quantitative radionuclide lung perfusion scan to see functional regional distribution but may
- not be available in all hospitals. This can be performed later in the
- LVR specialist centre.
- Echocardiogram to assess cardiac status particularly the right heart function.
- Arterial blood gases to ensure a range of PaO2 >7.0kPa and/or PaCO2 <7.0kPa
Bronchoscopic LVR
Patients may be considered for bronchoscopic lung volume reduction (BLVR)- endobronchial valves (EBV). EBVs have been developed to provide lung volume reduction and may be offered to patients with a higher chance of morbidity, patients not suitable for an invasive surgical approach or those not wanting to undergo a surgical excision.4
EBVs are less invasive than open or thoracoscopic LVR surgery as they are inserted via a bronchoscope with the patient under general anaesthesia or sedation.5 Several EBVs may be required for each segment of the lung to be treated.5 They are placed in the target areas of the lung, which results in lobar atelectasis (collapse or closure of the lobe resulting in reduced or absent gas exchange).
However, their success depends on the absence of collateral ventilation (allowing air to escape during expiration and preventing entry during inspiration, resulting in gradual lobar collapse). This is confirmed by analysing the CT scan for fissural integrity as well as on table Chartis assessment. EBVs are not successful if there is collateral ventilation and the patient may then have to be considered for a surgical LVR. The average in-hospital stay is approximately 72 hours – with complications such as bronchospasm, pneumothorax and valve removal reported.5 Treatment with EBVs in carefully selected patients has provided statistically significant benefits in lung function, exercise tolerance, dyspnoea and quality of life.5,6
Surgical LVR
Lung volume reduction surgery (LVRS) aims to surgically remove the worst parts of the emphysematous lung, in order to optimise the functionality of the healthier part of the lung, thus improving chest wall and respiratory muscle mechanics.4 Thoracoscopic volume reduction (some units still open procedures) is performed when the emphysema is isolated to certain areas of the lungs or varies between the segments of the lung (heterogeneous disease) this may allow for target areas to be removed surgically. Predominant upper lobe disease has been recognised as having the most beneficial and significant results of LVRS.4 LVRS is performed under a general anaesthetic by a thoracic surgeon using a keyhole approach (video assisted thoracoscopic surgery) and is usually performed on one side at a time.
Careful patient selection is paramount. Balancing the inherent risks associated with surgery and general anaesthetic in a patient with poor pulmonary reserve and/or physically deconditioned against the intended benefits is a key determining factor in patient outcome. The National Emphysema Treatment Trial (NETT) was a key study in validating LVRS as a safe treatment modality for COPD patients.7 In addition, it showed a survival benefit for patients with both predominantly upper-lobe emphysema and low base-line exercise capacity.
The average length of in-hospital stay is approximately ten days with the common complications reported as post-operative chest infections, respiratory failure and persistent air leaks from the lung.4
Referral process
A confirmed diagnosis of emphysema is required prior to referral to the LVR MDT to assess suitability for LVR. To be eligible for LVR MDT assessment, patients need to meet the following criteria:8,9
- Evidence of symptomatic chronic airway obstruction and hyperinflation with impaired quality of life.
- MRC dyspnoea scale > 3
- Non-smoker for 4 months
- Completed course of pulmonary rehabilitation within last 12 months.
- Body mass index (BMI) >18kg/m2
- Confirmed emphysema on high resolution computed tomography (HRCT) scan.
- Patients not suitable for assessment by LVR MDT are patients with:8,9
- Severe co morbidities-renal, hepatic or cardiac failure
- Severe progressive disease including disseminated malignancy
- Type 2 Respiratory Failure
- Severe Pulmonary Hypertension
Lung volume reduction multi-disciplinary team
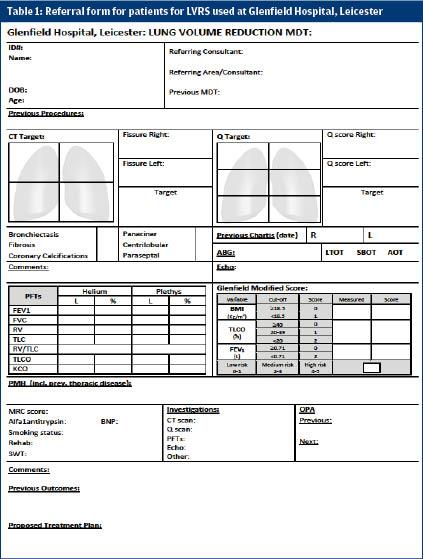
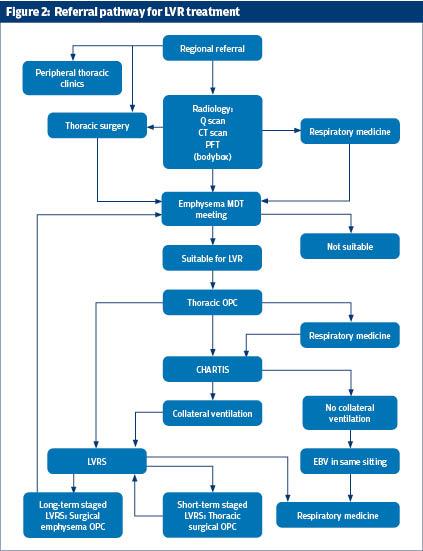
Within our centre all potential patients for LVR are referred to a specialised LVR multi-disciplinary team via pro-forma (see figures 1 and 2). The LVR MDT consists of respiratory physicians, a thoracic surgeon and a radiologist and meetings are held every 4 weeks. The LVR MDT reviews and assesses each patient using a standardised approach maintaining continuity in care and equity. The MDT looks for the presence and location of target areas. With the help of a CT scan the fissure integrity are determined. This will help with the decision whether the patient is suitable for EBV and/or VATS LVRS. Predictive risk scores such as the Glenfield BFG (body mass index, FEV1, gas transfer) score can be a useful tool in quantifying mortality risk associated with surgery in these patients.4
The National Institute for Clinical Excellence (NICE) recommends that all patients with emphysema should be managed by a multi-disciplinary team, however any suitable health care professional could perform an initial assessment (general practitioner, respiratory nurse, physiotherapist, occupational therapist etc) and should consider assessing the patient’s suitability for LVR.8
If patients are then deemed suitable the second assessment should be performed by a respiratory physician as part of the patients’ respiratory review. Not all patients with emphysema may be suitable for LVR and careful assessment may be required to assess suitability.
Some patients do not fit the requirements of the MDT as their pulmonary function may not have severe enough airway obstruction, or there may be an absence of target areas for resection, therefore these patients should continue to be managed by the respiratory physicians and can be reassessed if their respiratory function changes.
Patients are declined LVR if they have a lack of suitable target areas or if they carry an excessive risk of morbidity or mortality.8,9,10
Benefits of LVR
Results of LVR vary with individuals but has been recognised as improving lung function, exercise tolerance and quality of life in patients with this debilitating disease.9,10 The results of LVR may be short lived due to the nature of this progressive disease, but for some patients’ consideration may then be given to having further surgical intervention on the other side.
Long term success of LVR is affected by a number of factors including: non-dependence on oxygen supplementation prior to intervention; one year post-procedural improvement of FEV1 and pre-operative DLCO (diffusion capacity for carbon monoxide).11 The NETT long term follow up did demonstrate a survival benefit in patients undergoing LVR.7
Conclusion
Many patients may be suitable for LVR and yet many are still not referred for assessment by a lung volume reduction multi-disciplinary team. As health care professionals, we could ensure patients know there may be additional options to managing their disease and help facilitate the referral to a respiratory physician and subsequent LVR MDT to ensure all possible treatments have been explored.
Jayne Sharman, Advanced Nurse Practitioner, Glenfield Hospital, University Hospitals of Leicester
Kudzayi Kutywayo, Specialist Registrar, Glenfield Hospital University Hospitals of Leicester
Inger Oey, Clinical Fellow, Glenfield Hospital, University Hospitals of Leicester
Sridhar Rathinam, Thoracic Consultant, Glenfield Hospital, University Hospitals of Leicester
References
1. Munari AB, Gulart AA, Dos Santos K, Venancio RS, Karloh M, & Mayer AF. Modified Medical Research Council Dyspnea Scale in GOLD Classification Better Reflects Physical Activities of Daily Living. Resp Care 2018;63(1): 77-85.
2. Moorjani N, Viola N, Walker WS et al; Key Questions in Thoracic Surgery. Shrewsbury: tfm publishing; 2016. P475-492.
3. Disease G. GOLD COPD 2020 strategy [Internet]. Guidelines. 2020 [cited 26 March 2020]. Available from: https://www.guidelines.co.uk/respiratory/gold-copd...
4. Rathinam S, Oey I, Steiner M, Spyt T, Morgan M & Waller D. The role of the emphysema multidisciplinary team in a successful lung volume reduction surgery programme. Eur J Cardiothorac Surg 2014; 46:1021-1026.
5. National Institute for Health and Care Excellence. Endobronchial valve insertion to reduce lung volume in emphysema. 2017, Dec. Available from: www.nice.org.uk/guidance/ipg600
6. Lee E. & Rhee, C. Bronchoscopic lung volume reduction using an endobronchial valve to treat a huge emphysematous bullae: a case report. BMC Pulm Med 2019;19-92. Available from: https://doi.org/10.1186/s12890-019-0849-z
7. Fishman A, Martinez F, Naunheim K, Piantadosi S, Wise R, Ries A, Weinmann G, Wood DE; National Emphysema Treatment Trial Research Group. N Engl J Med 2003 May 22;348 (21)
8. National Institute for Clinical Excellence. Lung volume reduction surgery for advanced emphysema (Interventional procedures guidance). 2005, Feb 23. Available from: http://nice.org.uk/guidance/ipg114
9. NHS England. Clinical Commissioning Policy Proposition: Lung volume reduction by surgery or endobronchial valve for severe emphysema in adults. Available from http://www.engage.england.nhs.uk
10. National Institute for Health and Care Excellence. Chronic Obstructive Pulmonary disease in over 16s: diagnosis and management (G) Referral criteria for lung volume reduction procedures, bullectomy or lung transplantation. 2018, Dec. Available from: www.nice.org.uk ISBN: 978-1-4731-3175-0
11. Iwasaki, A & Yosinaga, Y & Kawahara, K & Shirakusa, T. Evaluation of Lung Volume Reduction Surgery (LVRS) Based on Long-term Survival Rate Analysis. The Thoracic and Cardiovascular Surgeon 2003. 51. 277-82. 10.1055/s-2003-43088.
