
The latest annual report of the Care Quality Commission, the regulator for health and adult social care in England, sounds the alarm. Here we have reviewed the report, State of Care 20231 and its impact on primary care.
Key findings
A year on from last year’s ‘gridlocked’ care and seven since the 2016 ‘tipping point’, the system is well and truly creaking under the aftermath of the COVID-19 pandemic, staffing shortages and record waiting lists of over 7 million. The Parliamentary and Health Service Ombudsman (PHSO) finds 'This report makes for extremely difficult reading.'2
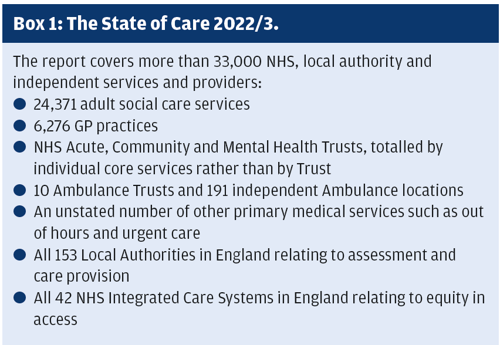
CQC’s report on over 33,000 NHS and independent providers of health and adult social care (Box 1) highlights the pressures on services right across the system. There is a strong focus on the impact of chronic staffing shortages which are ultimately increasing health inequalities on the 'slow slide to a two-tier' system,3 as people with funds pay for care while others wait.
Staff are dissatisfied. Only a quarter (26%) of NHS staff were happy with their pay, down from 38% before the pandemic. The resulting high turnover and vacancies impact people’s access to care and the quality of services delivered, particularly in maternity and mental health services.
Small changes in aggregated ratings for all providers do not overtly betray these changes, apart from maternity services where 49% are rated Requires Improvement or Inadequate, and in mental health and urgent and emergency care.4 The majority of provision overall continues to be rated ‘Good’.
In primary care, even with the drop of 1% in GP practices rated ‘Good’, (125), GPs retain the highest proportion of their services rated ‘Good’ (90%).
Access to care
The initial entry point to care, via GPs, is slow, explored below. Following GP referral, waiting lists for elective care total 7.6 million, the highest ever and 12% higher than last year. However, the true picture is likely to be higher as people wait longer for GP referrals. 'A chasm of inequality is growing in accessing care,' says the Royal College of Nursing (RCN).5
In A&E, over half (51%) of respondents to CQC’s urgent and emergency care survey waited more than an hour before being examined by a doctor or nurse, up from 28% last year.
Discharge from hospital is slow, due to the chronic lack of capacity in adult social care.
In residential and community services, people are at risk of not receiving the care they need, due to ongoing financial and staffing pressures.
As a result, people who can afford to are increasingly turning to independent services:
- 1 in 8 of 8000 surveyed by YouGov had used private healthcare in the last year
- More than half said they had used private healthcare to be seen more quickly.
Access to GP appointments
A lack of access to GP appointments is slowing referrals and eventual treatment, and masking the numbers waiting for care.
A survey by Healthwatch highlighted that:
- Four or more visits to the GP were needed before 1 in 5 (18%) of the 1500 people surveyed got a referral
- 11% waited over 4 months from the first GP appointment to the referral.
Half the 750,000 respondents to this year’s GP Patient Survey did not find it easy to get through on the phone. Once through, 16% of people then wait for more than 2 weeks for an appointment.
Of the 16% of people (120,000) unable to initially get an appointment, 32% found none available.
While local authorities and integrated care systems are responsible for reducing health inequalities in their areas, which increase as more people pay for care, effective measures and timeframes to enable this were not widespread.
Access to cancer care
Waits for cancer treatment continue to worsen. NHS England data show that 18,193 (40%) had waited more than two months to start their first treatment following an urgent GP referral, up from 22% in 2019.
This does not take account of hidden waits for cancer care. Almost half (45%) of the 385 adults expecting cancer treatment surveyed by Healthwatch were not referred for suspected cancer at their first appointment. More than a quarter (28%) also waited up to a month after their first appointment to be told they were being referred. Almost a quarter (23%) of people whose initial cancer referral was delayed reported their condition worsened as a result.
The impact on people waiting for care affects not only their health but also their wellbeing. A strong negative effect was reported by around a third of 2,524 Office for National Statistics respondents who were waiting to start NHS treatment.
The health and care workforce
Overstretched staff and insufficient staffing impacts on the quality of care that can be provided, as well as on the wellbeing of staff. This, despite the glimmer of green shoots:
- NHS FTE staff in hospital and community health trusts increased 5% in the year to May 2023
- Staff turnover there decreased from 13% to 11% in the year to June
- In general practice, FTE staff increased by 2.6% in the year to July 2023, although the number of GPs decreased by 1.2% and their turnover increased
- In adult social care, the number of FTE staff in post increased back to 2020/21 levels and turnover reduced from 37% to 29% in June 2023.
The Royal College of Midwives (RCM) has also recently estimated a shortfall of 2500 midwives.6
CQC make the close link between the right staffing numbers, skills and experience and achieving best outcomes for service users. The impact is significant, for example:
- Shift numbers not meeting the planned targets, resulting in risks to safe care including waiting for assistance and hands and face rather than full body washes
- Risks arising from inconsistent and/or unfamiliar staff supporting individuals due to high use of bank and agency
- Risks due to the lack of access to care including ‘closed’ beds due to staffing shortages
- Skills gaps leading to a lack of availability of some types of assessments
- The services’ ability to maintain training levels amongst staffing groups with high churn.
- Services are responding to staffing challenges. GP practices, for example, are increasing their use of complementary roles such as paramedics and advanced nurse practitioners, improving access without waiting for referrals or advice.
International recruitment is also growing, with some 70,000 people arriving from India, Nigeria, and Zimbabwe in 2022/3 to start direct care roles in adult care. International medical graduates (IMG) make up more than 40% of all GP trainees, although a third (30%) were considering no longer working as an NHS GP due to visa difficulties.
Reactions to the report
Responses to the report were swift and clear. The RCN noted the 'shocking state of care … from the cradle to the grave', and sees investment in the nursing workforce as the way forward.5
The RCM6 said the 'worrying picture of the state of maternity services', is not a reflection of staff’s dedication but of 'continued lack of investment in maternity services.'
The NHS Confederation called for a credible plan, 'after a decade of under-investment in staff, buildings and infrastructure.'7
The King’s Fund focused on the sad fact that health inequalities are rife and continuing. It calls for bold action from the government including reforming the model of social care and making health and care a more attractive career.3
The PHSO sees 'too much of the current provision is ineffective at assisting those who need care most.' It calls for a genuine learning culture in the NHS to become embedded, and for 'long-term workforce planning'.2
Conclusions
The regulator’s annual report again raises the roof on current concerns. It makes 'uncomfortable reading for the Government, with crises on multiple fronts.'7
While it includes a range of good examples, the overwhelming message is that most movement is going the wrong way. Plans are critically needed to inject life into services which have been under-invested for a decade, to address workforce recruitment, retention and development, and to reverse health inequalities.
Will next year’s report see much change? Proponents of the drive for integrated care, which will be within scope then following implementation of CQC’s new inspection regime, would say so. We watch and wait.
Amanda Halliwell, Independent care coach.
https://claritascarecoach.co.uk
amandaatclaritas@gmail.com
References
1. State of Care 2022/23 - Care Quality Commission (cqc.org.uk). Accessed 05 11 23
2. PHSO. https://phsombudsman-newsroom.prgloo.com/news/ombudsman-comments-on-cqcs-annual-state-of-care-report
3. Kings Fund. https://www.kingsfund.org.uk/press/press-releases/kings-fund-responds-annual-cqc-state-care-report
4. Appendix: CQC ratings charts - Care Quality Commission. Accessed 04 11 23
5. RCN. https://www.rcn.org.uk/news-and-events/Press-Releases/royal-college-of-nursing-responds-to-cqc-state-of-care-report-201023
6. RCM. https://www.rcm.org.uk/media-releases/2023/october/cqc-report-doesn-t-pull-any-punches-say-the-rcm/
20 10 23 Accessed 04 11 23
7. NHS Confed. https://www.nhsconfed.org/news/nhs-confederation-responds-cqcs-state-care-report
